Recently the ONC commissioned Accenture to develop a draft Whitepaper on PGHD, "Conceptualizing a Data Infrastructure for the capture, use, and the sharing of Patient-Generated Health Data in Care Delivery and Research through 2024". It is currently in draft and a good overview of the PGHD landscape.
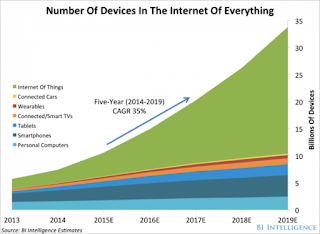
What I find lacking in the draft is the upcoming deluge of IoT information such as, home and workplace environmental data along with endpoints such as vehicle OBR (On Board Reporting), which impacts a person's health. It is predicted that we will have thousands of sensors providing bio and environmental data in the very near future. How and where are we going to store and provide access to this data? How will it be authenticated and secured? Will it become part of our medical record? Who will own and manage the data?
Much of this data will be near real-time streamed data which will need to be cleaned, compressed and analyzed. EHRs, which focus on the collection of clinical data do not have the ability or architecture to manage this high volume of non-clinical data. PGHD data is unstructured, it doesn't follow standards such as HL7 or LOINC to name a few, and is mostly stored in proprietary data sets. The data doesn't fall under HIPAA protection unless it is stored in an EHR raising the liability of the providers and organizations.
The growth cycle will probably need to be brought in two to three years based the current rapid development of sensors and IoT technology. This will future stress the EHR vendors to attempt to accommodate this data rather than focusing on their core business of providing an interface for providers to access patient data.
Security and privacy are a major concern with IoT sensors and devices. It takes an architecture that is built from the ground up to support remote client devices. A secure architecture which supports authorization, authentication, data-provenance, non-repudiation and transparency.
A new PGHD data architecture is needed to provide an interface between the EHR and the Patient's devices. A platform that can scrub, analyze and format results and findings for a provider to access via a portal or EHR. Health Record Banking may be the solution, a patient controlled standalone distributed database that is secure, accessible anywhere, anytime and anyplace,